Category
Uncategorized
Hypermetabolic Focal Fat Sparing
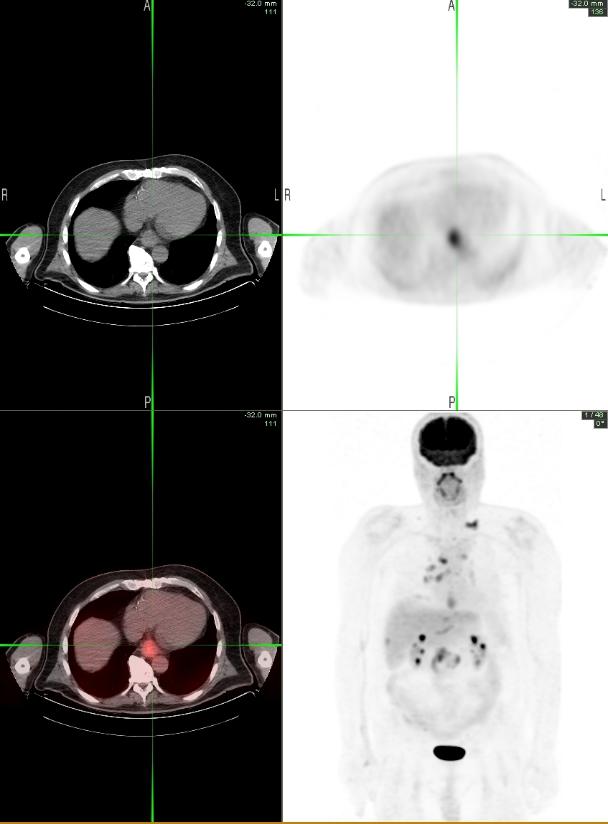
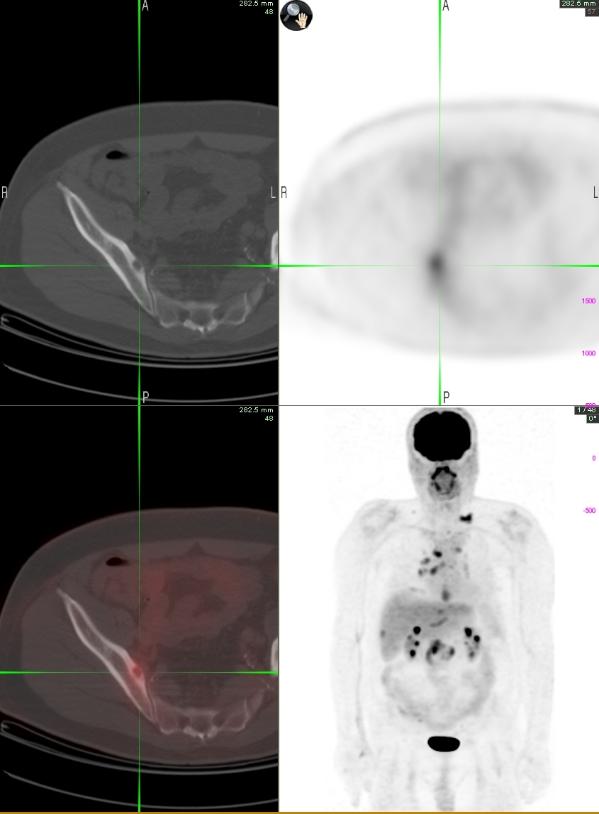
59 year old man with history of colon cancer (T4N0M0 – transverse colon mass with invasion of anterior abdominal wall, s/p extended right hemicolectomy with en block resection of proximal transverse colon and anterior abdominal wall) presented with fluid collection in the abdomen and pelvis, seen on a CT scan. Whole body PET-CT was done to assess for recurrent disease. Liver function tests were within normal limits at time of scan. PET-CT case of the month (04/10): Hypermetabolic Focal Fat Sparing

PET images show diffuse increased uptake in the left lobe of liver (SUVmax 3.0) and relatively decreased uptake in the right lobe of liver (SUV max 2.2). The corresponding CT images show that the low attenuation right lobe of liver (from fatty infiltration) is well demarcated from the normal looking left lobe of liver. Fat infiltrated liver is likely hypometabolic compared to the spared liver tissue. Focal fat sparing has been shown to mimic metastatic disease on PET-CT imaging (1).
1. Focal Fat Spared Area in the Liver Masquerading as Hepatic Metastasis on F-18 FDG PET Imaging. Purandare, N C.; Rangarajan, Venkatesh; Rajnish, Anshu; Shah, Sneha; Arora, Abhishek; Pathak, Sujata. Clinical Nuclear Medicine. 33(11):802-805, November 2008.
Lewy Body Disease
An 84 year old African American male with long history of memory difficulty and visual hallucinations, as well as, legal blindness presented to clinic for follow up. He has REM sleep behavior with occasional confusion and agitation during his sleep. His memory seemed to be stable for quite some time per his family. However, upon starting Aricept his visual hallucinations worsened. Aricept was subsequently discontinued. A head CT showed mild subcortical chronic ischemic in the subinsular region bilaterally. Dystrophic calcifications were noted in the right globe and along the right retina. Left scleral band was noted. A PET CT of the brain was ordered suspecting lewy body disease (LBD).
The F-18 FDG Brain PET-CT images show mild age appropriate atrophy with mildy decreased metabolism in the bilateral posterior temporo-parietal lobes and severely decreased metabolism in the bilateral occipital lobes. Normal metabolic activity is present within the frontal lobes, cerebellum, and the subcortical nuclei. These findings are highly suggestive of Lewy body disease (1). After Alzheimer’s disease, Lewy body disease is the second most common cause of senile degenerative dementia. Common symptoms include progressive cognitive dysfunction, psychotic symptoms (mainly visual hallucinations), parkinsonian motor signs (especially rigidity), and rapid cognitive fluctuations(2).

Clinical criteria Lewy body dementia has been delineated to allow clinical diagnosis (3). The clinical criteria provide excellent specificity (90–97%), but are lacking in sensitivity (only 22–75%) (4). Progressive debilitating mental impairment progressing to dementia is characteristic, however, this is common in many dementias. Impairments in attention, problem solving and visuospatial difficulties are early manifestations. Features which are helpful in differentiating Lewy body disease from Alzheimer’s disease include: fluctuations in cognitive function, spontaneous motor features of parkinsonism, and marked visual hallucinations (4). Previously autopsy was relied upon for the definitive diagnosis.
In this patient the diminished occipital uptake is likely due to Lewy body disease and not due to orbital pathology. A prior study performed on eight patients with congenital homonymous hemianopsia (seven with damage to optic radiations and one with optic tract abnormality; all with largely intact occipital cortex), showed minimal abnormalities in the resting visual cortex glucose metabolism of the “pathologic” visual cortex (5).
1. Mettler F., Guiberteau M. Essentials of Nuclear Medicine Imaging. 2006. p391
2. Mirzaei S, et al. Assessment of diffuse Lewy body disease by 2-[18F] fluoro-2-deoxy-D-glucose positron emission tomography (FDG PET). BMC Nucl Med. 2003 Feb 20. doi: 10.1186/1471-2385-3-1.
3. McKeith IG, et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology. 1996;47:1113–1124.
4. Ransmayr G, et al. Demenz mit Lewy-Körperchen. Nervenarzt. 2000;71: 929–935. doi: 10.1007/s001150050689.
5. Bosely TM, et al. Neuro-imaging and positron emission tomography of congenital homonymous hemianopsia. Am J Opthalmol. 1991 Apr 15; 111(3): 413-8.
This case was compiled by Bradley J. Potsic M.D, BCM
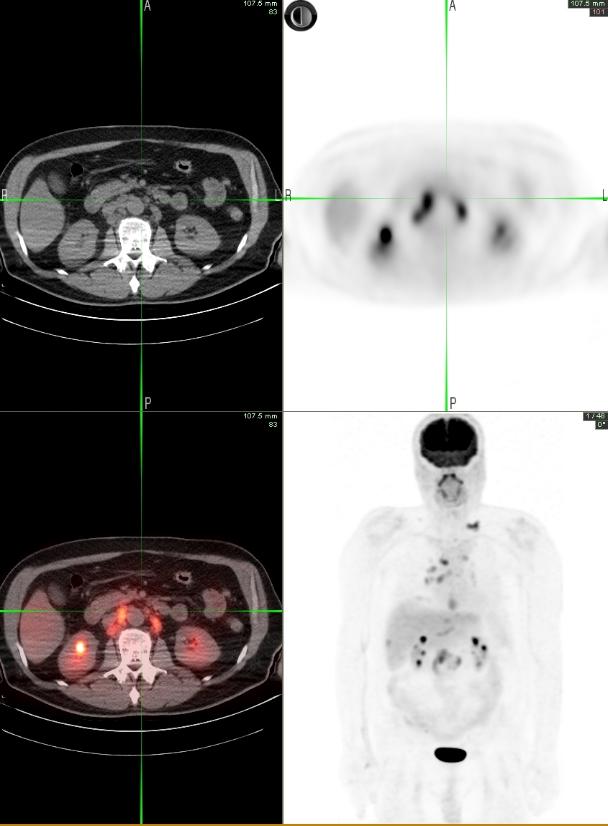
Lung Cancer and CLL
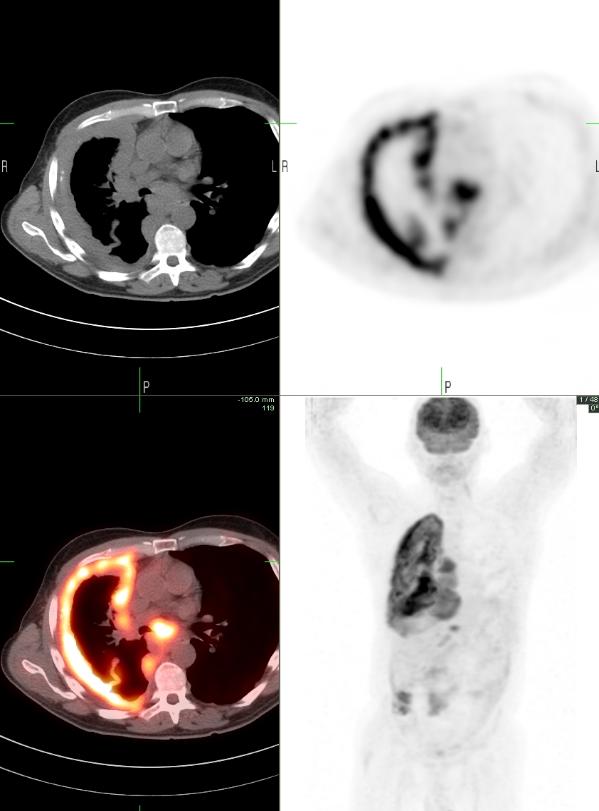
79 year old man with a history of bronchitis, diabetes, prostate cancer (s/p radiation therapy in 2000 and stable normal PSA), and chronic lymphocytic leukemia (since the 1970s, not treated and stable) presents with cough. Since 2009 his WBC count has been progressively increasing along with decrease in Hb/Hematocrit and platelet count. His Lymphocyte Doubling Time (HDT) is less than 12 months, predicting progression (1). Recent CT scan showed axillary, mediastinal, retroperitoneal, pelvic and inguinal lymphadenopathy, hepatosplenomegaly, and a new right upper lobe lung nodule, measuring 1.3 cm.
PET-CT show focal hypermetabolism in the right upper lobe lung nodule (SUV measuring 3.0) consistent with neoplastic involvement, likely a second primary lung cancer. CT-guided biopsy of the lung nodule showed squamous cell lung cancer and CLL. CLL is associated with a greater risk for a second malignancy such as lung cancer compared to the general population (2).


Mild hypermetabolism is also seen in the axillary and inguinal lymphadenopathy (SUV max of 2.2) suspicious for a low grade neoplastic process (CLL). A focus of hypermetabolism is also seen in the prostate (SUV measuring 3.3) which could be neoplastic or inflammatory.
1. Molica S and Alberti A. Prognostic value of the lymphocyte doubling time in chronic lymphocytic leukemia. Cancer 1987 Dec 1;60(11):2712-6.
2. Hisada M, Biggar RJ, Greene MH, Fraumeni JF Jr and Travis LB. Solid tumors after chronic lymphocytic leukemia. Blood 2001 Sep 15;98(6):1979-81.
This case was complied by Dr. Niraj Patel, BCM
Sarcoidosis
A 46 yrs old male presents with persistent abdominal pain for 1 yr. Abdominal CT found a soft tissue mass in the pancreatic tail and a hypodense liver lesion which was negative for malignancy on biopsy. Chest CT was performed before diagnostic laparoscopy with possible resection, and showed a left upper lobe nodule, mediastinal and hilar lymphadenopathy. PET-CT was performed for further characterization.
PET-CT images demonstrate symmetric increased FDG uptake in mediastinal and hilar regions (maximum SUV measuring 5.4), a pattern consistent with sarcoidosis The left upper lobe nodule did not show FDG uptake. Faint FDG uptake was seen in the pancreatic tail mass.

1. Sarcoid-like reaction to malignancy on whole-body integrated (18)F-FDG PET/CT: prevalence and disease pattern. Chowdhury FU, Sheerin F, Bradley KM, Gleeson FV. Clin Radiol. 2009 Jul;64(7):675-81.
2. Imaging features of sarcoidosis on MDCT, FDG PET, and PET/CT. Prabhakar HB, Rabinowitz CB, Gibbons FK, O’Donnell WJ, Shepard JA, Aquino SL. AJR Am J Roentgenol. 2008 Mar;190(3 Suppl):S1-6.
3. Bilateral hilar foci on 18F-FDG PET scan in patients without lung cancer: variables associated with benign and malignant etiology. Karam M, Roberts-Klein S, Shet N, Chang J, Feustel P.J Nucl Med. 2008 Sep;49(9):1429-36.
This case was compiled by Dr. David He, BCM
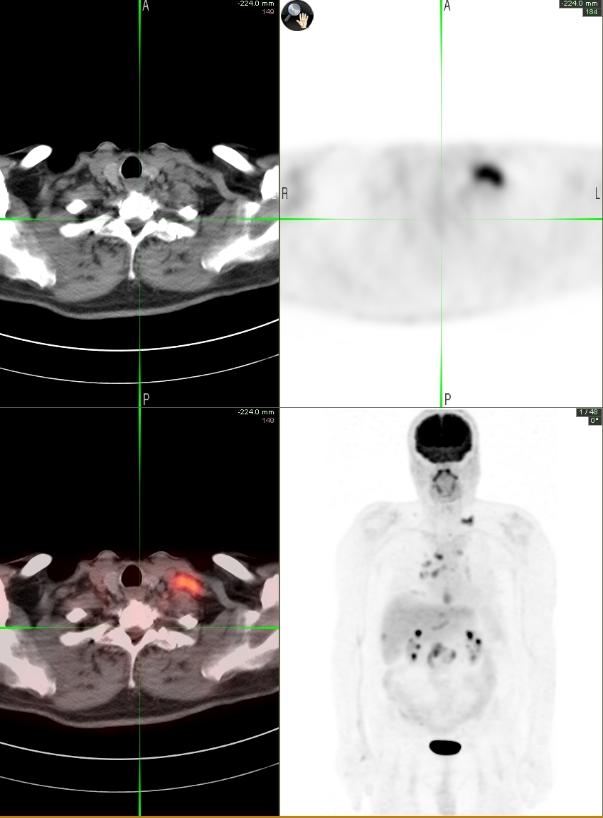
Head and Neck Cancer
73 yrs old male presented with painless left neck mass. A contrast enhanced CT of the neck showed necrotic left level II cervical lymphadenopathy concerning for metastatic disease, and a 1.7 x 1.5 cm mass arising from the superficial lobe of the right parotid gland. A 1.2 cm nodule was also visualized in the right lung apex. FNA of the enlarged cervical lymph node showed metastatic keratinizing squamous cell carcinoma.
Whole body FDG-PET CT showed asymmetric uptake in the left tonsil with a maximum SUV of 8.6. Hypermetabolic left cervical level II lymphadenopathy had a maximum SUV of 6.9. Indeterminate focal hypermetabolism was seen in the right parotid gland with a maximum SUV of 6.0. The right upper lobe pulmonary nodule also showed hypermetabolism (SUV 3.9) suspicious for neoplastic involvement.


Biopsy of the left tonsil showed squamous cell carcinoma and the biopsy of right parotid gland showed pleomorphic adenoma, a benign tumor.
The right upper lobe pulmonary nodule was biopsied and showed non small cell carcinoma with features of adenocarcinoma.
Thus, PET-CT localized the primary squamous cell carcinoma to left tonsil and diagnosed an incidental second primary malignancy in the lung

1. FDG PET and PET/CT for the detection of the primary tumour in patients with cervical non-squamous cell carcinoma metastasis of an unknown primary. Paul SA, Stoeckli SJ, von Schulthess GK, Goerres GW. Eur Arch Otorhinolaryngol. 2007 Feb;264(2):189-95.
2. The presentation of malignant tumours and pre-malignant lesions incidentally found on PET-CT. Even-Sapir E, Lerman H, Gutman M, Lievshitz G, Zuriel L, Polliack A, Inbar M, Metser U. Eur J Nucl Med Mol Imaging. 2006 May;33(5):541-52.
This case was compiled by Dr. Scott Lenobel, BCM
Extranodal Lymphoma
An 84 yrs old male with a past medical history of HTN and renal insufficiency presented with one month history of swelling in the right hard palate. He had difficulty lying on his right side due to pain but was otherwise asymptomatic. Biopsy of the lesion revealed large B-cell lymphoma. PET-CT was performed for whole body staging.
PET-CT showed hypermetabolic soft tissue masses in the: right hard palate (SUV 6.3), liver (SUV 8.0), and bilateral kidneys. Multiple bone lesions were also seen involving: focus in the sternum, the left 7th rib posteriorly, and the left transverse element of T8 vertebrae. No hypermetabolic lymphadenopathy was seen on PET-CT (extranodal lymphoma). Due to the unusual presentation liver biopsy was performed (to rule out a synchronous primary), which also showed large B-cell lymphoma.



Patient was treated with R-CVP (rituximab, cyclophosphamide, vincrisine and prednisone) with adriamycin added in the second cycle. PET-CT obtained post 2 cycles of chemotherpy showed complete resolution of all hypermetabolic lesions, suggesting good response to therapy.
1. Fluorine-18 fluorodeoxyglucose PET/CT patterns of extranodal involvement in patients with Non-Hodgkin lymphoma and Hodgkin’s disease. Even-Sapir E, Lievshitz G, Perry C, Herishanu Y, Lerman H, Metser U. Radiol Clin North Am. 2007 Jul;45(4):697-709
2. PET and PET/CT in management of the lymphomas. Podoloff DA, Macapinlac HA. Radiol Clin North Am. 2007 Jul;45(4):689-96.
3. Normal and abnormal patterns of 18F-fluorodeoxyglucose PET/CT in lymphoma. Bar-Shalom R. Radiol Clin North Am. 2007 Jul;45(4):677-88
This case was compiled by Dr. Sania Rahim-Gilani and Dr. David He, BCM
Metastatic Esophageal Cancer
A 63 years old male with past medical history of CABG presented with a 2-3 week history of dysphagia. He was able to localize a point in the region of his distal esophagus where solid foods were getting ‘stuck.’ He was able to drink some liquids but noted that they too were passing with increasing difficulty. An EGD was performed by GI and a circumferential mass was seen at the lower end of esophagus. Biopsy showed invasive moderately differentiated adenocarcinoma. CT scan showed the mass at the distal esophagus, and lymphadenopathy in the aorto-pulmonary window, adjacent to the celiac trunk and along the lesser curvature of the stomach. EUS could not be performed due to luminal narrowing. A whole body PET-CT was acquired for initial staging and to evaluate for distant metastasis.
PET-CT images show a hypermetabolic lesion in the distal esophagus consistent with malignancy. Hypermetabolic lymphadenopathy (max SUV 8.3) is seen in the abdomen and thorax, and also in the left supraclavicular region (Virchow’s node), consistent with metastasis. Multiple small hypermetabolic lesions are seen in the liver, suspicious for metastasis. A hypermetabolic and lytic lesion seen in the right ilium, and focal uptake seen in the left pedicle of T3 are consistent with bone metastasis.
1. The evolving role of PET-CT in the management of esophageal cancer. Chuang HH, Macapinlac HA. Q J Nucl Med Mol Imaging. 2009 Apr;53(2):201-9.
2. The role of 18F-FDG PET/CT in the evaluation of oesophageal carcinoma. Chowdhury FU, Bradley KM, Gleeson FV. Clin Radiol. 2008 Dec;63(12):1297-309.
This case was compiled by Dr. Sania Rahim-Gilani, BCM
Alzheimer’s Disease
A 64 year old male with memory problems for last seven years presents with severe progressive dementia. MRI of the brain showed moderate cortical volume loss and non-specific periventricular white matter changes secondary to small vessel disease.

F 18 FDG Brain PET-CT shows cortical atrophy and moderate to severely decreased metabolism in the bilateral posterior temporo-parietal regions, worse on the right. Mild decreased activity is also noted in the frontal regions. There is sparing of the sensori-motor cortex with normal distribution in the occipital region, sub cortical structures and the cerebellum.

Alzheimer’s’ disease or Dementia of Alzheimer’s type (DAT) is strongly suggested in this patient due to the classic finding of reduction in the bilateral posterior parieto-temporal regions and sparing of the sensorimotor cortex. Decreased metabolism in the frontal regions is suggestive of advanced Alzheimer’s disease.
In early Alzheimer’s diseases, PET findings relate to hypometabolism in the bilateral parietotemporal regions, which can often be asymmetric. In more advanced disease, the frontal lobes also show decreased FDG uptake. CT and MRI show ventricular and cortical atrophy, which has been used to diagnose DAT, but studies have shown that PET is more sensitive than MRI or CT to detect cortical involvement in dementia.
1. Franz Fazekas, Abass Alavi et al. Comparison of CT, MR, and PET in Alzheimer’s Dementia and Normal Aging. JNM 1989; 30: 1607-1615.
This case was compiled by Dr. Sabeen Rahman (BCM)
Mesothelioma
61 yrs old male presented with c/o productive cough for 3 months. He was initially treated with antibiotics for possible pneumonia, but without success. Subsequent chest CT found extensive pleural based soft tissue density encasing the right lung with possible mediastinal and diaphragmatic invasion, suspicious for mesothelioma.
PET-CT images show intense linear FDG uptake surrounding the right lung and extending into the right hemidiaphragm, corresponding to the soft tissue density on CT, max SUV measuring 9.5, consistent with mesothelioma. Multiple hypermetabolic nodes seen in the mediastium and the upper abdomen are consistent with metastatic disease.

1. The role of positron emission tomography/computed tomography in the diagnosis of pleural diseases. Orki A, Akin O, Tasci AE, Ciftci H, Urek S, Falay O, Kutlu CA Thorac Cardiovasc Surg. 2009 Jun;57(4):217-21.
2. 18F-fluoro-2-deoxy-D-glucose positron emission tomography and positron emission tomography/computed tomography imaging of malignant pleural mesothelioma. Subramaniam RM, Wilcox B, Aubry MC, Jett J, Peller PJ. J Med Imaging Radiat Oncol. 2009 Apr;53(2):160-9
3. Morphologic and functional imaging of malignant pleural mesothelioma. Yamamuro M, Gerbaudo VH, Gill RR, Jacobson FL, Sugarbaker DJ, Hatabu H Eur J Radiol. 2007 Dec;64(3):356-66.
This case was compiled by Dr. David He (BCM) and Dr. Joji Varghese (MEDVAMC)
Pulmonary Tuberculosis
A 58 year old caucasian male, nonsmoker, with h/o hypertension and gout presents with shortness of breath. He has lost 20 lbs of weight in the last 2 yrs which he attributes to life stressors and poor appetite and endorses having had long-term asbestos exposure.
Chest Xray showed bilateral non-specific nodular lesions and pleural effusion. CT scan of the chest showed bilateral pulmonary nodules suggestive of metastatic cancer or infection, right lower lobe mass, bilateral pleural effusion, worse on the right, and a large hypodense soft tissue mass in the lower abdomen. No evidence of mediastinal or hilar adenopathy

The transbronchial biopsy was positive for chronic inflammation and AFB. A sputum sample was sent for culture and showed pan-sensitive TB. Patient was started on Directly Observed Therapy (4 drugs – for 9 months). Follow-up CT showed no change in the original pulmonary nodules, decrease in size of the right lower lobe mass and slight decrease in the pleural effusion. Patient improved clinically.
Follow up PET/CT showed significantly decreased FDG activity in the lung lesions, along with a generalized decrease in size, suggesting a good response of pulmonary TB to the 4-drug therapy.

1. Evaluation of therapeutic response of tuberculoma using F-18 FDG positron emission tomography. Park IN, Ryu JS, Shim TS. Clin Nucl Med. 2008 Jan;33(1):1-3
2. Usefulness of 18F-fluorodeoxyglucose positron emission tomography for diagnosing disease activity and monitoring therapeutic response in patients with pulmonary mycobacteriosis. Demura Y, Tsuchida T, Uesaka D, Umeda Y, Morikawa M, Ameshima S, Ishizaki T, Fujibayashi Y, Okazawa H. Eur J Nucl Med Mol Imaging. 2009 Apr;36(4):632-9